Patients are often taken by surprise when told by their doctor that they have just been diagnosed with type II diabetes. The news can be particularly shocking and unexpected because this form of the disease does not usually manifest until the individual is older (after age 45), and is more commonly seen in people who lead a sedentary lifestyle and/or have a family history of diabetes.
Patients are forced to face the reality that is the disease. Increased risk for stroke, heart disease, kidney problems and nerve damage are just some of the risks that individuals must confront as they work with their healthcare team to manage their blood sugar, ultimately aiming to lower their risk for the aforementioned complications.
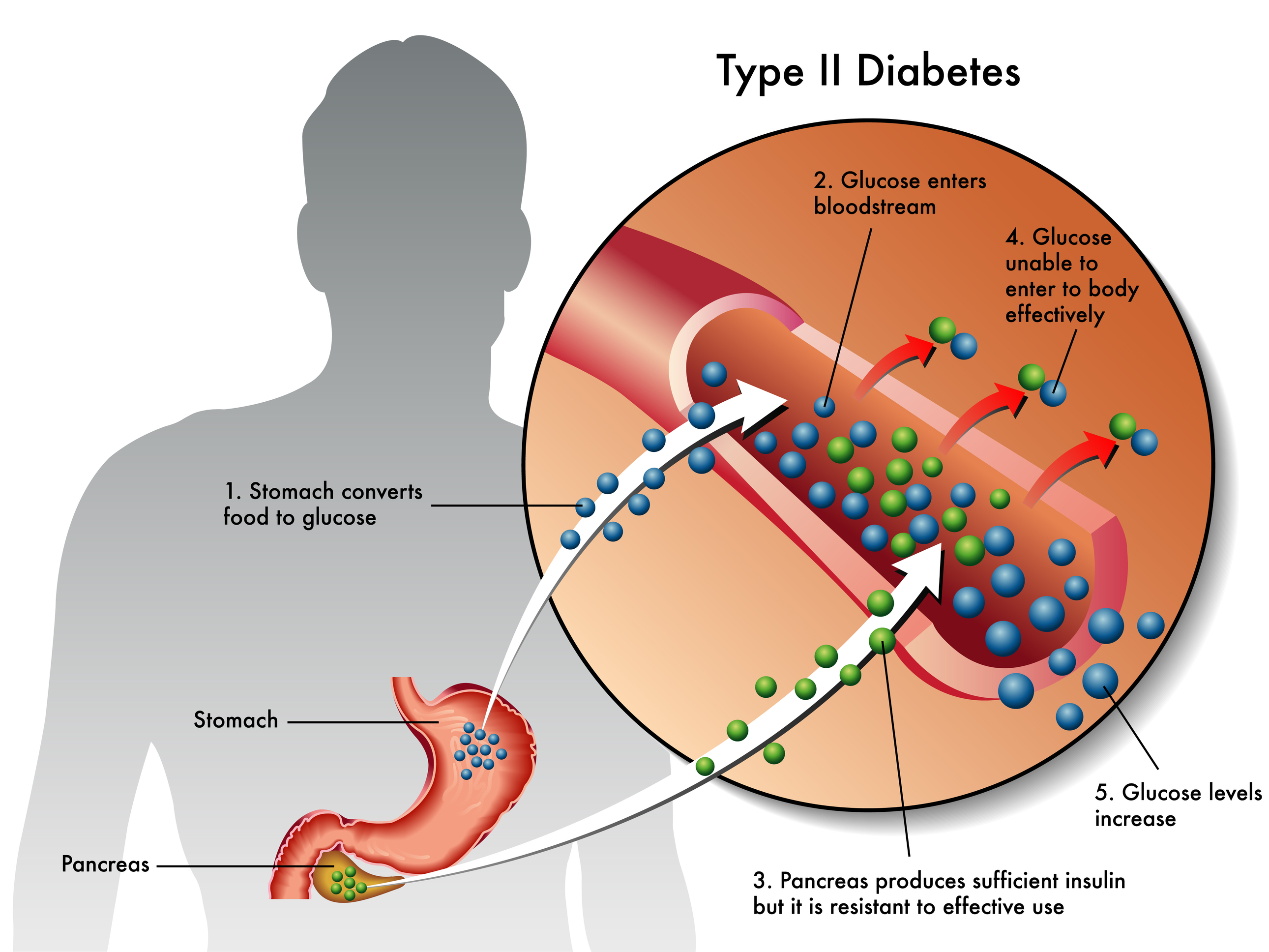
In a healthy individual, after food is digested, the sugar is removed from the blood by a hormone called insulin, which is released by the pancreas. The insulin is the key to the door, which allows glucose to enter the cells so it can be converted into energy. In type II diabetes, the pancreases produces and releases insulin, but the cells of the body are not sensitive to it and therefore are unable to accept the glucose. This defective process causes the glucose to remain in the bloodstream, as it builds, negatively impacting the patient's health.
Remember that you're not alone and that with a proper diet and exercise program, you can take control and manage this disease. Getting in the habit of checking blood sugar levels and taking the steps to manage it can be a tough learning experience. Endocrinologists recommend following the guidelines below, after an assessment with your doctor.
Work with your Health Care Team
Working with an endocrinologist, diabetes expert and/or dietitian is important, especially for a Type II diagnosis to determine how many carbohydrates, fats and proteins should be consumed each day, and at which times. The consumption of foods that are healthy and keep levels of sugar in the blood steady should be heavily incorporated into the diet.
Consider Beginning Treatment with Medication
At least initially, until you better understand how to manage the disease and control blood sugar, consider taking medication. Metformin is the most commonly prescribed med for an initial defense against the dangers associated with high blood sugar. Once you are able to control your levels with exercise and diet, you will be able to slowly come off the medication under supervision of your doctor.
Quit Smoking
More than likely, you will be asked by your doctor to quit smoking cigarettes immediately, since smoking constricts blood vessels and individuals with diabetes are at risk for decreased blood flow to the feet which can result in the loss of limbs. Quitting is the best way to avoid these complications.
Get Enough Physical Activity
If you don't like to exercise at a gym, there are other ways to stay active such as bike riding, walking, hiking and dancing. According to the CDC, adults need at least 2 hours and 30 minutes of moderate-intensity aerobic activity (e.g., brisk walking) every week and muscle-strengthening activities on 2 or more of those days. You can find more information here.
Exercise and Eat Right
Individuals with type II diabetes in particular can greatly benefit from exercise, diet and increased physical activity. Checking blood glucose levels at home (using a glucometer) and recording, is an effective way to learn how your body responds to various foods and lifestyle changes. The goal is to keep blood glucose levels steady and low. Learn what works for you, and in no time you will get into healthier habits.
Manage Your Weight
One of the goals of treatment is to educate the individual on techniques to lower and ultimately control blood glucose levels. The long-term goal is to prevent or minimize health issues from diabetes by managing blood glucose levels. By managing their weight, individuals will be able to reduce the levels of glucose in the blood. Acquiring a lower body fat percentage will cause the cells in the body to become more sensitive to insulin, so glucose will have an easier time entering the cells as it should.
See your Physician for Routine Checkups
Having diabetes increases your risk for nerve damage of the feet, and issues with vision. Yearly eye and foot exams are important to help avoid damage to these areas. Foot exams help prevent nerve damage, infections and damaged blood vessels.
Even if you are taken by surprise by your diagnosis, lots of help is available to get you on track to control your type II diabetes and keep you there.